The three major growth factors are genetic, nutritional and hormonal. The hormones that are essential for a normal growth process are growth hormone and insulin-like growth factor I (the key), thyroxine, cortisol and sex steroids.
Ten essential questions from murtagh
1. Is the child actually short ?
2. Is the child short compared with other children?
3. Is the child unexpectedly short from a genetic viewpoint?
4. Is the child's growth slowing ?
5. If the growth is slow, what is the reason?
6. How dose the child feel about the short stature?
7. How does the height percentile match against a growth velocity chart?
8. Has puberty commenced?
9. Is there any specific investigation warranted?
10. Is there any specific therapy warranted?
The causes of short stature can be grouped into the following categories:
1. Organic causes
2. Constitutional delay
3. Familial short stature
Examination
1. General inspections includes dysmorphic features and nutritional status. Measure all anthropometry (height, weight, GV, upper/lower segment ratio) and compare with percentile charts
2. Measure skeletal proportions
3. Assess pubertal status
Investigations
If GV is < 25th percentile for bone age, consider
- TSH
- FBE and ESR
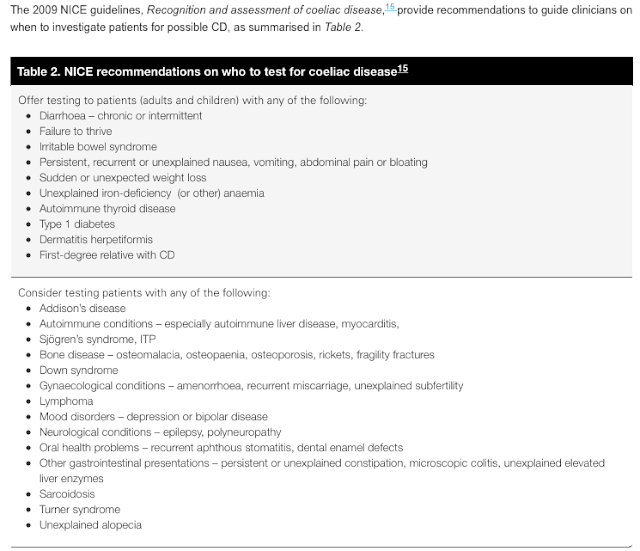
- Coeliac disease
- Chromosomes in all girls. Karyotype to exclude Turnes 45 XO
- Growth hormone studies: IGF - 1
- Kidney function
- Bone age x-ray (left wrist)
Management:
- May require growth hormone
References:;
John Murtagh
http://www.rch.org.au/uploadedFiles/Main/Content/MedEd/fracp/short%20stature%20NEJM.pdf